Infections and Dental Implants
Infections and dental implants go hand in hand when it comes to dental health. While dental implants herald a revolution in restorative dentistry, their potential vulnerability to infections cannot be overlooked.
This guide explains the relationship between dental implants and infections, emphasising the critical aspects of risk factors and preventive measures.
What Are The Common Causes Of Infections After Dental Implants?
Infections after dental implants in Dubai often arise due to bacteria entering the implant site during or after surgery. Some common contributors of potential infections can be contamination, poor oral hygiene, or pre-existing dental conditions.
Cause | Explanation | Prevention |
Bacterial Contamination | Bacteria introduced during surgery | Sterile surgical environment |
Poor Oral Hygiene | Inadequate cleaning of mouth | Regular brushing & flossing |
Compromised Immune System | Weakened body defences | Maintain general health |
Pre-existing Conditions | Gum diseases predisposing to infections | Address before implant surgery |
Improper Implant Placement | Incorrect positioning can trap bacteria | Experienced dentist placement |
Tobacco Use | It hampers healing and invites bacteria | Avoid tobacco |
This table provides a quick overview of the common causes of dental implant infections, their explanations, prevention methods, and the severity of their risks.
How Can Infections Impact The Success Of Dental Implants?
Infections can compromise the osseointegration process, where the implant fuses with the jawbone, potentially leading to implant failure.
- Disruption of Osseointegration: An infected site can prevent the implant from securely bonding with the jawbone.
- Bone Loss: Infections can lead to bone deterioration around the implant.
- Implant Mobility: An infected implant might become loose over time.
- Prolonged Healing: Healing duration can extend due to infections.
- Implant Failure: Severe infections can result in the complete failure of the dental implant.
- Additional Surgical Interventions: Infected implants often require more surgical treatments.
What Are The Early Signs Of An Infection Around A Dental Implant?
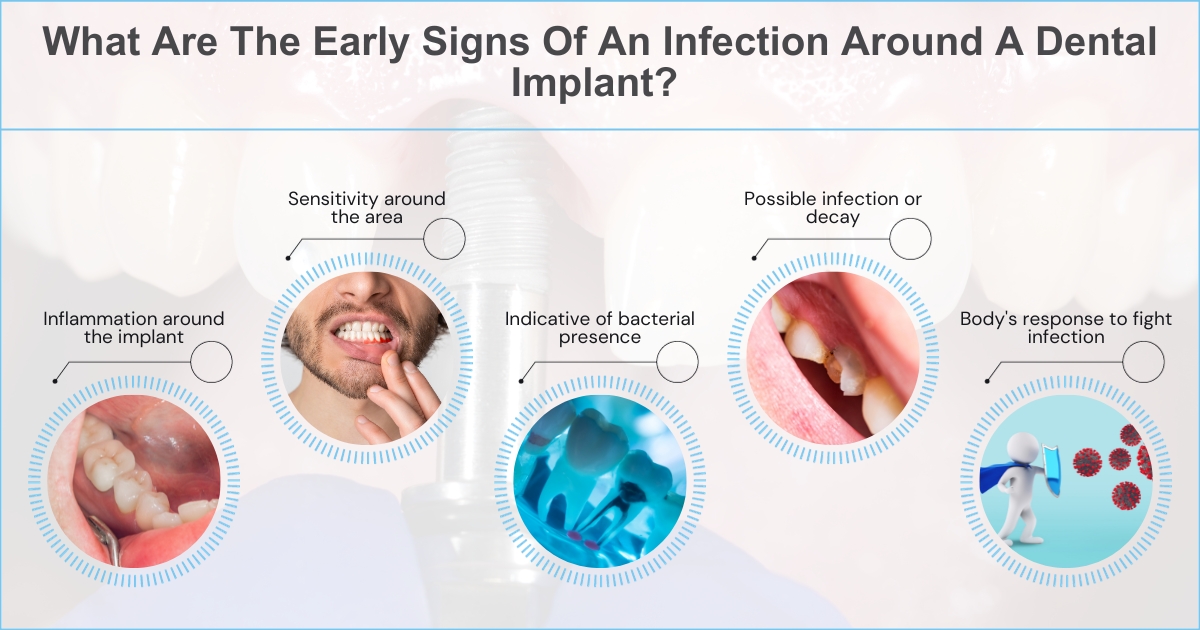
Early signs of an infection after a dental implant include redness, swelling at the implant site, pain or discomfort, pus discharge, and a bad taste or odour in the mouth. If you experience any of these symptoms, immediately consult your dentist to ensure prompt treatment and prevent further complications.
Sign | Explanation | Immediate Action |
Redness & Swelling | Inflammation around the implant | Consult dentist |
Pain or Discomfort | Sensitivity around the area | Monitor & seek medical advice |
Pus Discharge | Indicative of bacterial presence | Begin antibiotic treatment |
Bad Taste or Odor | Possible infection or decay | Oral cleaning & check-up |
Fever | Body’s response to fight infection | Seek medical attention |
Difficulty in Chewing | Tenderness when pressure is applied | Check implant positioning |
The table above showcases the early signs of a potential infection around a dental implant, explains their significance, and suggests immediate action.
How Often Do Dental Implants Get Infected?
While dental implants boast a high success rate, infections can occur in a minority of cases, typically due to poor oral hygiene or surgical contamination.
- Dental implants have a very low infection rate, typically between 4% and 10% for postoperative infection.
- The infection rate is higher for certain types of implants, such as zygomatic implants and transmandibular implants.
- The infection rate is also higher for patients with certain health conditions, such as diabetes and smoking.
- Early detection and treatment of infection is important to prevent further damage to the implant and surrounding tissues.
Can An Infected Dental Implant Be Saved?

Yes, with timely intervention and treatment, many infected dental implants can be saved, although severe cases might require removal.
Treatment | Explanation | Success Rate | Timeframe |
Early Detection | Identifying symptoms early on | High with timely action | Immediate |
Antibiotic Treatment | Combatting bacterial infections | Moderate to High | Days to Weeks |
Deep Cleaning | Professional cleaning around the implant | Moderate | Immediate to Days |
Surgical Intervention | Procedures to address severe infections | Variable | Weeks to Months |
Implant Removal | In case of irreversible damage | N/A (implant is removed) | As needed |
This table presents the various treatments for infected dental implants, giving a brief description, their success rates, and the expected timeframe for action or recovery.
How Does Oral Hygiene Play A Role In Preventing Implant Infections?

Good oral hygiene eliminates bacterial buildup, which prevents infections and ensures dental implants’ longevity.
Here are some tips for maintaining good oral hygiene around dental implants:
- Brush your teeth twice a day for two minutes each time.
- Use a soft-bristled toothbrush and fluoride toothpaste.
- Floss your teeth once a day.
- Use a mouthwash specifically designed for dental implants.
- See your dentist for regular checkups and cleanings.
Are There Specific Types Of Bacteria Responsible For Dental Implant Infections?
Here are some specific types of bacteria that are responsible for dental implant infections:
- Actinomyces: This type of bacteria is found in the mouth and throat. It can cause infections of the gums, jawbone, and other tissues around dental implants.
- Porphyromonas gingivalis: This bacteria is a major cause of gum disease and periodontitis. It can also cause infections of dental implants.
- Prevotella intermedia: This type of bacteria is often found in dental plaque. It can cause infections of the gums, jawbone, and other tissues around dental implants.
- Fusobacterium nucleatum: This bacteria is found in the mouth and gut. It can cause infections of the gums, jawbone, and other tissues around dental implants.
- Streptococcus mutans: This bacteria is a significant cause of tooth decay. It can also cause infections of dental implants.
What Treatments Are Available For Infections Around Dental Implants?
Treatments include antibiotic prescriptions, improved oral hygiene practices, deep cleaning around the implant, and, in severe cases, surgical interventions.
Treatment Option | Purpose | Duration | Effectiveness |
Antibiotics | Address bacterial infections | Days to weeks | High with early detection |
Implantoplasty | Smoothen implant surfaces to deter bacterial colonisation | Single session | Moderate to high |
Laser Therapy | Reducing inflammation and bacterial count | Multiple sessions | Effective with early infections |
Surgical Debridement | Remove infected tissues around the implant | Single session | Moderate to high |
Implant Removal | In cases of severe, unresolvable infections | As needed | N/A (implant is removed) |
Regenerative Procedures | Rebuilding bone or gum tissue lost to infection | Multiple sessions | Varies based on severity |
This table introduces treatments available for addressing infections around dental implants, detailing their specific purpose, typical duration, and effectiveness.
How Long After Getting A Dental Implant Can Infections Occur?
Infections can occur shortly after the surgery or even years later. However, immediate post-operative infections are more common.
Timeframe | Risk Level | Cause | Preventive Steps |
Immediate (0-2 weeks) | High | Surgical contamination | Sterile surgical environment |
Short-term (2 weeks – 3 months) | Moderate | Poor post-operative care | Follow aftercare instructions |
Medium-term (3-12 months) | Low to moderate | Delayed healing or foreign body reaction | Regular check-ups |
Long-term (1 year+) | Low | Poor long-term oral hygiene | Consistent oral hygiene routine |
The table represents the infection risks at different times post-dental implant surgery, specifies common causes for each period, and recommends preventive measures.
What Role Does The Quality Of The Dental Implant Play In Infection Risks?
High-quality dental implants made from biocompatible materials reduce the risk of infections and promote better integration with the bone.
- Biocompatible Materials: These reduce the chances of infections and allergic reactions.
- Quality Manufacturing: Premium implants have smoother surfaces, reducing bacterial adhesion.
- Professional Placement: Proper placement by an experienced dentist minimises risks.
- Longevity: High-quality implants tend to last longer and face fewer complications.
Can Infections Spread From Natural Teeth To Dental Implants?
Yes, infections from natural teeth, significantly if they’re affected by periodontal disease, can spread to neighbouring dental implants.
- Periodontal Disease: This is a primary concern for implant infections.
- Proximity Matters: Implants close to infected natural teeth are at a higher risk.
- Bacterial Migration: Bacteria can move from natural teeth to implants.
- Regular Dental Cleaning: This can prevent the spread of infections.
- Awareness of Oral Health: Understanding one’s dental health can prevent complications.
Being proactive is the key to understanding the dynamic between infections and dental implants. With the right precautions, the effectiveness of dental implants can be upheld, affirming their long-term advantages.
For personalized guidance on dental implants, schedule a consultation with NOA Dental Clinic Dubai. Your oral health deserves expert attention.
Frequently Asked Questions About Infections and Dental Implants
High-quality implants reduce infection risk due to superior materials and fit.
Treatments range from antibiotics to surgical interventions, depending on the severity.
Not always; early detection and treatment can save the implant in many cases.
Look for signs like redness, swelling, discomfort, or unusual discharge around the implant.
Crucial, as they allow early detection and address potential complications.

